

 The Father of Hip Replacement Surgery The modern method of hip replacement surgery was invented in 1962 by Sir John Charnley, an orthopedic surgeon from Wrightington, England. Charnley’s work was one of the greatest advances of 20th century surgery. Two revolutionary features of his technique were the use of polymethyl methacrylate bone cement to attach the artificial components of the replacement hip stem to the bone and the use of a metal ball and stem with a plastic socket. The plastic socket offered very low frictional resistance and a low wear rate against the metal ball. Knee and shoulder replacement techniques were also developed as a direct result of Charnley’s work. Today the stem portions of most hip implants are made of different alloys. They also come in different shapes and use different design features. But the overall design of the device and the surgical method Charnley developed are basically the same. Although a different procedure than hip replacement surgery, hip fracture repair can be just as invasive. Research at the University of Notre Dame is contributing to dramatic changes in the hip fracture repair procedure, cutting surgical time and drastically reducing the length of both the initial hospital stay and rehabilitation. |
Biomechanics The Biomechanics and Biomaterials in Orthopaedics Group at Notre Dame is comprised of researchers from several departments within the College of Engineering, as well as from other sectors of the University and industry. “One of the benefits of being at Notre Dame,” says James J. Mason, associate professor of aerospace and mechanical engineering, “is location. Three of the five largest orthopedics companies in the country are headquartered in Warsaw, Ind., less than an hour away from the University. Several of our graduate students, and even undergraduates, travel to Warsaw on a regular basis to work with the orthopedics teams there.” A majority of the current research in biomechanics and biomaterials is the result of a partnership with Zimmer, Inc., a world leader in the design, manufacture, and distribution of orthopedic implants and fracture management products. In addition to working with Zimmer, College of Engineering researchers collaborate with faculty from Purdue University and Indiana University Medical School on other projects, a number of which are funded by Indiana’s 21st Century Research and Technology Fund, the National Science Foundation, and the National Aeronautics and Space Administration. Mason and Steven R. Schmid, associate professor of aerospace and mechanical engineering, have lead the University’s efforts in orthopedic research, garnering more than $4 million in funding for orthopedic implant research in the last two years. The majority of those projects include the design of devices that promote minimally invasive orthopedic implant surgery (MIOIS). While many of the group’s projects concentrate on the biomechanical aspects of MIOIS, several focus on the biomaterials and bioinformatics also needed as part of diagnoses and treatment procedures.  Consider the almost 350,000 hip fractures recorded each year with more
than 90 percent of those fractures occurring in people 65 and older.
In one of the most common fracture repair procedures, an orthopedic surgeon
makes a six-inch incision in the side of the patient, just over the hip
and thigh. This incision cuts through muscle tissue, nerves, and blood
vessels, exposing approximately six inches of the side of the femur.
A screw is driven through the bone into the head of the femur, which
acts as the ball of the hip’s ball-and-socket joint. A plate is
then attached to the side of the femur. Consider the almost 350,000 hip fractures recorded each year with more
than 90 percent of those fractures occurring in people 65 and older.
In one of the most common fracture repair procedures, an orthopedic surgeon
makes a six-inch incision in the side of the patient, just over the hip
and thigh. This incision cuts through muscle tissue, nerves, and blood
vessels, exposing approximately six inches of the side of the femur.
A screw is driven through the bone into the head of the femur, which
acts as the ball of the hip’s ball-and-socket joint. A plate is
then attached to the side of the femur.Because the incision cuts through so much muscle and other soft tissue, the leg is substantially weakened, causing instability and requiring lengthy rehabilitation times. For example, today all hip fracture patients require walking aids during the several-week to several-month rehabilitation process after surgery. Approximately 50 percent of those people need a cane or walker permanently, and 40 percent of all of the patients require ongoing nursing home care. Other serious complications from the surgery can also arise, largely due to the a patient’s decreased level of activity. Yet, this type of structural reinforcement to strengthen fractured bones, such as hips, has been employed and has remained relatively unchanged for decades. A hip fracture implant and surgical procedure developed as a result of the collaboration between Zimmer and Notre Dame offers hope. The new implant device and surgery requires only a one to two-inch incision and avoids cutting through the muscle, nerves, and blood vessels. The curable, metallic polymer components of the device, which provides the same strength as traditional implants, will be located in the canal of the femur. By avoiding the dissection of much of the area around the ball-and-socket joint, the leg should maintain the same stability and strength after the surgery as it had before the fracture. All in all, the new implant and procedure are expected to significantly reduce surgical recovery time, increase mobility immediately following the surgery, decrease rehabilitation time, and offer a much greater chance of resuming a normal level of activity after the surgery, which, in turn, will decrease the risk of pulmonary and other serious complications.  “Because of our successes to date, we have other orthopedic implants
in the works,” says Schmid. “All of our projects follow the
philosophy of being minimally invasive, not causing the patient a lot
of pain or physical trauma. The idea is that joint replacement should
be about as painful as getting a wisdom tooth pulled. Even working on
the projects, it’s hard to grasp the scope of what we’re
doing, because the pain level patients experience, the way surgeons treat
patients, and the outcome of many types of surgery are about to change
forever.” “Because of our successes to date, we have other orthopedic implants
in the works,” says Schmid. “All of our projects follow the
philosophy of being minimally invasive, not causing the patient a lot
of pain or physical trauma. The idea is that joint replacement should
be about as painful as getting a wisdom tooth pulled. Even working on
the projects, it’s hard to grasp the scope of what we’re
doing, because the pain level patients experience, the way surgeons treat
patients, and the outcome of many types of surgery are about to change
forever.”A second MIOIS project within the group involves spinal fixation. Current treatment methods call for the removal of the ruptured disc, which compromises the strength of the spine. Thus, at the same time they remove the disc, surgeons often attach a system of steel rods, retainers, and screws to the spine, covering the weakened area. The metal rods must be bent by the surgeon and then manually threaded through the stationary retainers to properly support the spine. Many patients, when confronted with the probable side effects of the surgery -- paralysis, numbness, or loss of function of the lower extremities -- decide to live with the pain of a ruptured disc. Although relying on the same procedure of drilling screws into the vertebrae to hold a supporting “bar,” the Notre Dame group, in collaboration with Zimmer, has developed a new device to replace the steel rod. A prefilled bag of liquid polymer will snap quickly and easily onto the screws. The surgeon will then apply either a plastic curing agent or ultraviolet light to begin the curing process. This method locks the spine into place with little stress on the spine or spinal column. Another aspect of biomechanics being explored in the College of Engineering is the mechanical behavior of bone, particularly cancellous bone which supports joints and is the type of bone most affected by osteoporosis and osteoarthritis. “Instead of studying metal or traditional structural elements, we’re studying the mechanical properties of bone,” says Glen L. Niebur, assistant professor of aerospace and mechanical engineering. “We’re trying to determine how bone, especially the porous bone around joints, responds to loads. What causes it to break? Why do bones break more easily as people age? And, if bone is damaged, does that affect its strength?” According to Niebur, what the group is doing is extending the boundaries of traditional engineering, working directly with biologists, biophysicists, and physicians to answer questions that no single group can answer alone. One of the devices Niebur uses is a high-resolution micro-computed tomography system, one of approximately 20 machines of its kind in the United States, to study the structure and strength of both normal and osteoporotic bone. The system used by Niebur is a modified version of a hospital CT scanner that is able to image structural features 100 times smaller than a hospital’s system.  “Actually,” says Niebur, “bone is a great material to work
with. It’s self-repairing. We also know that it is very oriented,
much stronger in one direction than another. It’s like trying to
break an egg from the ends, which is very difficult. We believe the repair
process works in this same ‘direction.’ If we can understand
how this works and the mechanics of it, perhaps we can find a way to
prevent osteoporosis rather than just treat it.” Niebur is working
on this project with JoEllen J. Welsh, professor of biological sciences.
The collaboration, he believes, is successful because it builds on the
strengths of engineering and biology to quantify their research. “We’re
trying to advance the state of human knowledge,” he says. “The
information we uncover will be put into the public domain to help other
researchers, as well as physicians, help people.” Niebur and colleagues
believe that the information gained through this research will ultimately
lead to better designs for medical devices and more effective treatment
methods for all types of bone disorders. “Actually,” says Niebur, “bone is a great material to work
with. It’s self-repairing. We also know that it is very oriented,
much stronger in one direction than another. It’s like trying to
break an egg from the ends, which is very difficult. We believe the repair
process works in this same ‘direction.’ If we can understand
how this works and the mechanics of it, perhaps we can find a way to
prevent osteoporosis rather than just treat it.” Niebur is working
on this project with JoEllen J. Welsh, professor of biological sciences.
The collaboration, he believes, is successful because it builds on the
strengths of engineering and biology to quantify their research. “We’re
trying to advance the state of human knowledge,” he says. “The
information we uncover will be put into the public domain to help other
researchers, as well as physicians, help people.” Niebur and colleagues
believe that the information gained through this research will ultimately
lead to better designs for medical devices and more effective treatment
methods for all types of bone disorders.As Notre Dame’s biomechanics and biomaterials group has grown, it has added faculty members with expertise in machining and shape optimization, in the design of machines -- for testing prostheses and other medical implants -- and in the characterization and creation of materials for use in surgical procedures. Three new faculty members were added last year. Additional faculty and expanded research funding are expected in the next academic year. |
|
|
|
The Biomechanics and Biomaterials in Orthopaedics Group This interdisciplinary team explores the interfaces between mechanical engineering, biomedical engineering, materials science, and biology. Projects focus on both basic and applied research and various aspects of experimental and theoretical solid mechanics, manufacturing, materials processing and characterization, tribology, biomedical imaging, and design. DEPARTMENTS Aerospace and Mechanical Engineering James J. Mason, associate professor Glen L. Niebur, assistant professor Timothy C. Ovaert, professor John E. Renaud, associate professor Ryan K. Roeder, assistant professor Steven R. Schmid, associate professor Michael M. Stanisic, associate professor Computer Science and Engineering Danny Chen, Rooney associate professor Patrick J. Flynn, associate professor Chemical Engineering Davide A. Hill, associate professor Chemistry and Biochemistry Marya Lieberman, assistant professor PROJECTS Biomaterials Anisotropic Damage of Cancellous Bone Anisotropy in Human Cortical Bone Application of Metal Foams in Orthopedics Bone Cement in New Orthopedic Procedures Continuum Properties of Cellular Solids Hydroxyapatite Whisker Reinforced Composites for Load-bearing Orthopedic Devices Multi-parameter Mechanical Characterization and Scratching of Polymers Synthesis of Anisometric Hydroxyapatite Particles Variable Diameter Fibers (VDFs) as a Novel Reinforcement in Biocomposites Biomechanics Anisotropic Damage of Cancellous Bone Anisotropy in Human Cortical Bone Bone Marrow Flow in Cancellous Bone Continuum Properties of Cellular Solids Multi-parameter Mechanical Characterization and Scratching of Polymers Shape Optimization in Orthopedics and Biomechanics Staining Techniques for Micro-CT Imaging of Microdamage in Bone Biomedical Imaging Minimally Invasive Orthopedic Implant Surgery (MIOIS) Shape Optimization in Orthopedics and Biomechanics Staining Techniques for Micro-CT Imaging of Microdamage in Bone Orthopedic Devices Application of Metal Foams in Orthopedics Bone Cement in New Orthopedic Procedures Hydroxyapatite Whisker Reinforced Polymer Composites for Load-bearing Orthopedic Devices Minimally Invasive Orthopedic Implant Surgery (MIOIS) Shape Optimization in Orthopedics and Biomechanics Variable Diameter Fibers (VDFs) as a Novel Reinforcement in Biocomposites FACILITIES Biomaterials Processing and Characterization Laboratory Design Automation Laboratory Nano-mechanical Characterization and Tribology Laboratory Solid Mechanics Laboratory Surface Science Laboratory Tribology/Manufacturing Laboratory http://www.nd.edu/~amebio |
 Boning up on the Stats ... • Nearly 350,000 hip fractures occur in the United States each year. Four percent of those people undergoing hip fracture repair surgery die during their initial hospital stay. Twenty-four percent of those over 50 years old die within one year of surgery. Close to 40 percent of the total number of patients require long-term care, and half of them never walk unassisted again. • More than 90 percent of all hip fractures in the United States each year occur in people 65 and older and are often associated with osteoporosis. • Of the total number of hip fractures that occur each year, 90 percent are the result of a fall. • By the year 2050, the American Association of Orthopaedic Surgeons estimates the number of fractures rising to 650,000 per year, nearly 1,800 per day. • The average cost of hip fracture care in America today is $33,000 per patient. -- American Association of Orthopaedic Surgeons, 2001 |
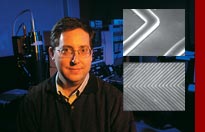 No one bats an eye when discussions on “wireless technology” include
telephones, computers, or satellites. But an inductively-powered
wireless system for monitoring blood in which the chemical sensors
are fabricated as microwave components ... that’s a different
story. For two years
No one bats an eye when discussions on “wireless technology” include
telephones, computers, or satellites. But an inductively-powered
wireless system for monitoring blood in which the chemical sensors
are fabricated as microwave components ... that’s a different
story. For two years